Keratoacanthoma is a self limiting, epithelial prolieration with a strong clinical and histopathologic similarity to well differentiated squamous carcinoma. Some consider it as a Cutaneous lesion presumably arise from the infundibulum of hair follicles. Intra Oral lesions are rare but have been seen.
It is a common low grade malignancy that origanates in the pilo sebaseous glands. It is also called as the “Self healing carcinoma”
It resembles Squamous cell carcinoma, and considered a variant of invasive squamous cell carcinoma.
Synonyms:
- Self healing carcinoma
- Molluscum pseudocarcinomatosum
- Molluscum sabecum
- Verrucoma
Differential diagnosis:
- Actin keratosis
- Molluscum contagiosum
- Muir-Torre Syndrome
- Squamous cell carcinoma
- Verrucous
Etiology:
- Exposure to sunlight
- Exposure to Pitch, tar.
- Trauma
- Human Papilloma Virus
- Genetic factors
- Immunocompramised status
Clinical Features:
Clinically it appears as a painless well circumscribed dome or bud shaped tumor of 1-2 cm in diameter with a keratin crater at the center. The tumor begins as a small nodule that grows rapidly and within 4-8
- Age: All ages are equally affected.
- Sex: M>F
- Race: White>Black
- Common sites on Body: Seen mostly in sun exposed areas- Face, neck, dorsum of upper limb.
- Common sites on face: Lips, Vermillion border.
- Lesions are Solitary, Firm, Round, Skin coloured (or) Reddish papules which progress to Dome shaped nodules with a shiny surface and a central crateriform ulceration (or) Keratin Plug that may project like a Horn.
- Lesions: Elevated Umbilicated (or) Crateriform with a depressed central core.
- Size: 1 – 1.5 cm in diameter.
- It is a painful lesion seen with Lymphadenopathy.
Course of the Lesion:
Small firm nodule –> Full size in 4 to 8 weeks –> (6 – 8 weeks in a static stage) –> Regrussion by expulsion of keratin.
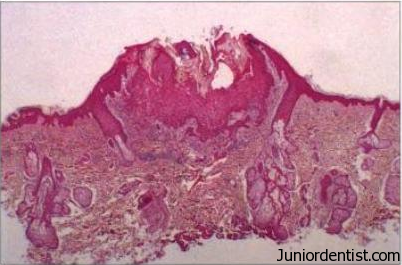
Histological features:
- Hyperplastic squamous epithelium can be seen growing into the underlying connective tissue.
- Surface is covered be Ortho keratinized or Parakeratinized epithelium with central plugging.
- At the margins the normal epthelium is elevated to the central portion of the crater, then an abrupt change in the normal epithelium occurs as the hyperplastic acanthomatous epithelium is reached.
- Borders / Margins are very important for diagnosis.
- At margins islands of epithelium appear invading the deep leading margin of the tumor.
- Pseudocarcinomatous infiltration typically presents a smoother, regular well demarcated front that does not extend beyond the level of sweat glands.
- Connective tissue shows chronic inflamatory cell infiltration.
Treatment and Prognosis:
- Surgical Exision.
- Aggressive therapy on recurrance.
- Recurrance is rare.
- Prognosis is good.
- May lead to skin cancer in future.